Tissue Healing and Electrotherapy – What, when, why?
Published:7 January,2020
by Helen Walsh, BSc, MCSP, HCPC, Clinical Lead U.K. & Ireland
Courtesy of Animal Therapy Magazine Issue 18
I’m in and out of professional sports teams these days and get asked many questions on electrotherapy (or electro physical agents (EPA’s) as we’re now calling them). A lack of time to update oneself continuously on tissue repair and the evidence base is contributing to myths surrounding certain modalities. Some people just outright ‘believe’ that they do nothing, despite a huge volume of research to the contrary. Companies also do a good job of confusing us, ‘proving’ their device is the answer to all our prayers offering quick fix solutions, when really it does not suit every injury or problem.
Let’s be honest here, there isn’t much that’s completely brand new in electrotherapy. Companies do an excellent job of making it seem like a new product when in fact it’s a reinvention of something old. It just looks better and not like some of those dust covered scary looking devices I’ve seen lurking in dark corners of a hospital therapy unit!
One of the main issues I come across on my visits is a lack of fully understanding the modality, when its best used and for what conditions. I am going to make a bold statement here; animal therapists do seem to have a better understanding than those therapists working with just humans (don’t shoot me!)
In this article I am going to attempt a whirlwind tour through tissue healing, with what to use and why. I am basing it on evidence, which comes from both the published resource and my own personal experience.
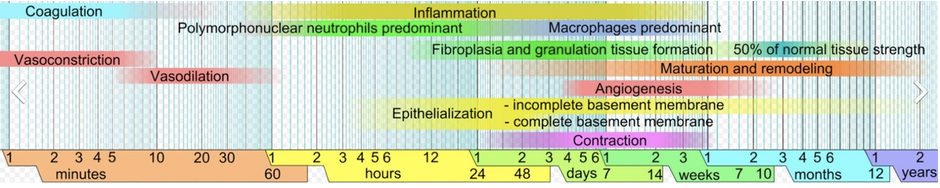
In figure 1, it gives a complete overview of what is occurring when and the overlapping of the different activities. I think of it as an orchestra, it all starts off with just one group, the flutes, slowly building tempo and sound, as other instruments join in. It builds to the crescendo of them all playing at once followed by a slowing down of tempo and instruments towards the end as they quietly go about their business.
Figure 1. Wound healing phases (1).
The difficulty with trying to simplify anything is that there will always be occasions when the injury is more severe and therefore spends more time in any of the above stages. As a therapist it’s up to us to determine a likelihood of where it’s at. This is through taking a history of the injury and in our assessment. Working with vets and having access to any diagnostic imaging of the case you are treating is very useful if not essential.
Stage 1- BLEEDING
Time: up to 6 hours approximately Treatment: ICE 10 minutes on 10 minutes off
From the table we can see that during those first minutes the body is attempting to limit blood loss. Vasoconstriction and coagulation take precedence during the first 10 minutes. Once there is enough coagulation to reduce bleeding the body triggers vasodilation.
In that first 6 hours the only intervention is ICE. However, this should not be left in place longer than 10 minutes. Time and again I’ve seen people strap it on and leave it during this period. The evidence has not changed regarding ice, it’s still only 10 minutes on and leave it off for at least 10 minutes.
Stage 2- INFLAMMATION
Time: 6 hours- 3 days (this is ongoing for longer, as it starts crossing over with proliferation we treat differently) Treatment: Non-thermal progressing to mild thermal
Inflammation is NORMAL and NECESSARY. It’s got some serious bad press, we’ve been saying ‘anti- inflammatory’ for a long time. There is a point that it can become chronic and that’s the one we don’t want but in an acute injury we absolutely want it.
For this reason, many including myself have been using the word ‘pro- inflammatory’. Let’s try and speed it along its way but not fundamentally ‘change’ it.
If you have the opportunity to treat at this point, the aim of treatment is to accelerate the normal process. As you move into this phase the intervention starts of with any of the non-thermal modalities depending on what it is that’s injured and how deep it is.
Stage 3- PROLIFERATION
Time: starts 24-48 hours after injury but peaks 2-3 weeks later Treatment: Increase blood flow
Fibroblasts start early on after injury. They play a role in angiogenesis (formation of new capillaries). It is an aerobic process and thus the increase in blood flow supports the delivery of oxygen to support it, especially in tissues that do not have a good blood supply.
We can influence this in several ways, mechanotransduction (aka exercise) can also support this process. Being selective at what exercise you start and ensuring that the healing isn’t completely disrupted by an excess of it. Other ways to influence a greater influence in blood flow can be through the use of EPA’s. The thermal inducing ones and the electric muscle stimulators.
Stage 4 – REMODELING
Time: 1st week up to 1 year Treatment: Heat, stretching, exercises, massage
This is massively important to us therapists to achieve a well-organised scar that behaves as much like the tissue of the structure that it has repaired. You can have very positive influences on this stage even months after an injury. Never underestimate how long it can take something which has been damaged to fully repair and have the same strength it had before. Always be aware that the older a patient the longer things take!
What modalities do we have at our disposal?
We may only have one or two of the below. Some do more than others and you should always see if it fits with what you see week in week out! You definitely want something that can help with a majority and earns its place in your toolbox paying for itself in time!
Disclaimer: I do keep abreast of current evidence I also talk to a lot of therapists which always helps when writing a guide. I do work for INDIBA which is an electromagnetic radiofrequency device. I have tried to be as unbiased in this as possible. I will always answer honestly about electro-physical agents.
Pulsed shortwave therapy (PSWT): (also known as PEME; pulsed electromagnetic energy, although this is not the ideal name) has very good evidence for wet/boggy tissue; muscle, hematomas, pain. The devices normally operate at 27.12MHz There are now smaller devices that can be used at home for longer periods of time. They are a good alternative to buying a huge device but you need to be aware of depth of penetration and dose (length of time) as they need to be left on for much longer to achieve a beneficial effect. It’s a very useful little gadget for in between sessions especially if you can’t get back out to them and they don’t cost much to keep a couple in your bag just in case.
Pulsed and non-pulsed laser (LLLT & LILT, photobiomodulation): the main consideration of using any ‘light’ based therapy is that hair and skin are barriers. Its also been found that darker skin can block out even more of the energy by scattering and absorption. This has been found by hundreds of research papers. If it’s a wound on skin or in the first 15mm with hair/skin colour not causing more of a barrier then laser is an excellent choice.
The difference between Class 3b and 4 in simple terms; a Class 4 can deliver more energy in less time. It does not go deeper, despite what the company say. There is also no evidence yet showing that the mitochondria further down will take the energy deeper into the body. The issue has always been that laser works where it reaches brilliantly, it does nothing more than you just looking at it, anywhere it cannot reach. Therefore hair, skin and what your trying to treat really matter with this type of energy delivery. It can be delivered in non-thermal and thermal doses and the heat can be a nice addition.
Be wary of very expensive ones claiming they go deeper and do your homework if purchasing. Ask for a trial and look at what actual results you get in the outcome measures.
Pulsed electromagnetic fields (PEMF) : I’d throw it out there that this is one of the most highly confused areas of EPA’s. It is not surprising, the complexity of the interaction of electricity and magnetism can have us baffled within minutes, especially when even the evidence has a multitude of parameters with quite a few not stating all the information needed.
In soft tissue injury, I’m not currently convinced (you may be and that’s fine!) that the best way is by wrapping the limb and having the magnetism around it. The evidence is patchy. I do think there is enough supporting pain relief though. However, one thing that does strike me is that sufficient magnetic therapy needs to be delivered in order to achieve therapeutic results. Again, penetration depth of the therapy can quite often be superficial even when left on for long periods, as in the study by Steyn 2000 where the measurement at 7mm from the wrap showed no difference to the earth’s magnetic field (2). Quiz the company on all the parameters and review the evidence for dosing.
Ultrasound: I almost feel like it doesn’t need to be in the list. I’d guess it’s the most well-known. It’s cheap and easy to understand and there is a plethora of evidence to support its use, think ligaments and tendons. You can be very superficial, and you can go a little bit deeper. It’s considered a non-thermal treatment because you will feel nothing. It doesn’t reach warm temperatures. In terms of fractures the evidence is very good. So much so you can get one on the NHS for delayed union (if your lucky, it is on NICE guidelines). Sports people use ultrasound to speed up fracture healing and do very well with it. Again, there are numerous companies selling devices so do your research and make sure it actually does do what it says on the tin.
Radiofrequency electric currents (RFEC): In all honesty I have put this last because I clearly work for INDIBA which is a RFEC device. Confusion can arise with this technology from it being an electromagnetic current at a particular radiofrequency, INDIBA is 448KHz and currently the majority of evidence has been at RF 448KHz. The most ‘like’ it would be pulsed short wave, however there is a big difference, the delivery is a direct electric current into the body which passes all the way through the body with some exiting via a neutral return plate. Recall above we mention magnetic with the coil on the outside, the magnetism here is accompanying the electric current through the tissues. The second part of confusion is that it can sit under the electrical stimulation title even though there is no muscle contraction, it can also deliver a thermal treatment to temperatures of 42 degrees and it can be non-thermal. This is the only one that I am aware of that goes very deep as it travels to wherever the neutral electrode is placed, and it is the only one that the evidence states will maintain an increase in tissue temperature for at least 45 minutes (3). All other modalities stop when the treatment stops. The limitation on this device is that the equine device (VET905) is a bit heavy, it certainly will build your muscles. The small animal device (AH-100) is super light. Again ask questions of the company and trial before you buy (I know you’d be convinced anyway like I was).
That was a whirlwind tour through some modalities that can help in tissue healing. Apologies for not exploring everything! For anyone wanting more information there is a lot online, a quick Pubmed search will keep you busy for hours on the topic! Professor Tim Watson does have a new book released recently; Electrophysical agents: Evidence based practice. In this, there are plenty of updates on the last, as is the way with evidence, it keeps growing and hopefully informs our practice to achieve better outcomes.

Related content:
INDIBA vs. OTHER EPAs: Differences in depth reach and why is it important
Sources:
- Mikael Häggström (2014). “Medical gallery of Mikael Häggström 2014”, WikiJournal of Medicine, 1 (2), doi:10.15347/WJM/2014.008, Wikidata Q44276778
- Steyn, 2020. Effect of a static magnetic field on blood flow to the metacarpus in horses.
- Kumaran, B; Watson, T (2015). Thermal build-up, decay and retention responses to local therapeutic application of 448 kHz capacitive resistive monopolar radiofrequency: A prospective randomised crossover study in healthy adults. International Journal of Hyperthermia, 31:8, 883-895, DOI: 10.3109/02656736.2015.1092172